레이더 센서를 활용한 의료용 IoT 디바이스 제작에 대해 인피니언 테크놀로지스(Infineon Technologies) 기술진으로부터 들어본다.
“레이더 센서, 비접촉 의료 IoT 혁신 이끈다”
AI·센서 융합, 병원·가정 등 건강 관리 환경 구축
XENSIV™, 16㎟크기 컴팩트 디바이스 설계 가능
의료 분야로 원격 생체 신호 모니터링을 위해서 간결하면서 에너지 효율이 우수한 레이더 센서를 찾는 수요가 빠르게 증가하고 있다.
▲그림 1 : 수면 모니터링
중중 질환 대상자가 아닌 일반 환자의 경우, 다중 생체신호(예 : 호흡 + 심박) 모니터링으로 사망 및 이상 증상 사례에 대해 최대 75% 예방 할 수 있다고 한다.[1]
특히 환자와 노인 의료에 있어서 중요한 측면이 호흡수와 심박수 같은 생체 지표를 모니터링하는 것이다.
ECG와 산소포화도 측정기 같은 검사 장비는 줄에 달린 전극을 직접 피부에 부착해야 한다.
뿐만아니라 케이블이 길게 이어지고 수시로 충전을 해야 해서 환자의 자유로운 이동이 제한될 수 있다.
하지만 개선된 에지 형태(edge-type) 레이더의 등장으로 새로운 비접촉식 생체신호 모니터링 방식이 가능하게 되었다.
이에 따라 비접촉 측정에 의한 지속적 생체신호 모니터링과 이상 증세 조기 감지 등의 장점을 바탕으로 가전제품 및 IoT 제품에 손쉽게 사용되고 있다.
이 글에서는 레이더 센서가 어떻게 환자의 치료를 향상시키는지 설명하고, 앞선 레이더 센서 기술로서 인피니언의 XENSIV™ 60GHz 레이더 센서를 소개한다.
■ 레이더 센서에 대한 이해
레이더 센서는 RF 신호가 전자기파 형태로 방출되며, 공간상에서 빛의 속도로 움직이면서 공간상의 사람과 사물에 의해 반사된 신호에 의해 미세한 움직임까지 감지하면서 이를 바탕으로 종합적인 모티터링 활동이 가능하다.
이를 위해 FMCW(Frequency Modulated Continuous Wave : 주파수변조 연속파) 레이더는 인체의 미세한 움직임을 측정 및 감지를 위해 사용 될 수 있고, 주파수 변조를 사용하면서 주파수 변화량 분석을 통해 정확한 거리와 속도를 측정 할 수 있다.
이어지는 내용으로 레이더 센서를 활용한 생체 신호 모니터링의 정확한 메커니즘을 살펴 보도록 한다.
■ FMCW 레이더 센서를 활용한 생체 신호 측정
레이더 센서는 호흡 중 흉강의 움직임을 감지 할 수 있는데, 이는 호흡 과정의 흉강 움직임 변화량에 의해 발생되는 레이더 반사 신호에 대한 미세한 차이를 감지한다.
이를 ‘레이더 기반 호흡 감지’ 기술이라고 부른다. 이에 대해 기본적인 작동 메커니즘을 살펴 보도록 한다.
FMCW 레이더는 시간의 흐름에 따라 RF신호를 연속적으로 방출하면서 주파수를 상승하고 하강하는 변조를 진행하게 되는데, 이러한 변조에 의해 반복적으로 일정한 주파수 대역의 파형을 만든다.
이 변조된 레이더 신호는 표적(흉강)을 향해 방출되고 그 일부가 반사되어 레이더 수신부로 되돌아 오는데, 반사된 에코라고 불리는 신호는 표적의 거리와 속도에 대한 유용한 정보가 담겨있다.
FMCW 레이더는 주파수를 선형적으로 변조된 파형을 방사하면서 반사된 신호 파형과 비교하게 된다.
이 과정에서 ‘Beat’ 혹은 중간 주파수(IF)가 만들어 만들어지는데, 이는 감지하고자 하는 물체의 거리와 상관관계를 갖는다.
즉 송수신 신호사이의 주파수 차이인 중간 주파수(IF)를 정밀하게 측정함으로써 거리측정 정확도를 크게 개선 될 수 있다.
다시 말해, 중간 주파수(IF) 측정의 정밀도에 의해 측정 거리의 정확도가 향상된다.
■ 비접촉 생체 측정 모니터링의 이점
○ 환자의 안전 향상
전통적인 유선 모니터링 시스템은 심전도와 산소포화도 센서들을 사용해서 심박수와 호흡수를 측정한다.
또한 줄에 달린 전극을 피부에 부착하기 때문에 피부 자극을 일으킬 수 있다. 민감한 환자들에게는 특히 더 그럴 수 있다. 뇌전증이나 정신과적 질환을 겪는 환자들에게 불안을 일으킬 수도 있다.
반면에 레이더 센서는 내장된 안테나를 사용해서 흉벽의 위치와 속도를 추적함으로써 생체 지표를 비접촉으로 측정할 수 있다.
안테나가 호흡과 심장 박동을 추적하고 정확한 생체 지표를 알려준다. 비접촉 측정 방식이므로 환자를 제약하거나 구속하지 않는다.
그러므로 환자를 불편하게 하거나 피부 자극을 일으키지 않는다.
○ 환자의 편의성
충분한 수면시간 하의 수면다원 검사는 전통적인 폐쇄성 수면 무호흡 증상에 대해 높은 비용과 첫날 밤 효과(FNE-first night effect) 같은 제한이 있다[9].
특히 관찰 대상에 대한 낙상의 경우는 잠재적으로 오동작를 발생 시킬 수도 있다.
하지만 이 레이더 센서는 어떠한 외부 신호와 무관하게 자체적으로 반사신호에 의해 대상을 감지하며, 비금속 물질을 투과할 수 있기에 최종 제품의 외장 커버 뒤에 비노출식 사용이 가능하다.
○ 정확도와 신뢰성
전통적인 ECG는 심박 측정을 위해서 인체에다 전극을 부착한다. 이러한 전극들은 환자를 불편하게 하고 개인의 자연스러운 호흡 패턴을 교란함으로써 측정되는 생체 지표로 부정확성을 야기할 수 있다.
이와 달리, 비접촉 생체 신호 모니터링은 환자가 측정을 의식할 필요가 없기에, 호흡 변동 가능성이 낮아 생체신호 측정 정확성을 향상시킬 수 있다.
또한 기존의 ECG는 전극을 피부에 부착하면서 피부를 압박한다. 그럼으로써 전기적 특성을 변화시키고 측정되는 신호로 부정확성을 초래할 수 있다.
하지만 레이더 센서는 비접촉으로 측정하기 때문에 인체에 어떠한 압박을 가하지 않는다. 이에 따라 탐지되는 신호가 본연의 생물학적 작용 상태에 근사하며, 이를 통해 정확한 생체 신호 측정을 가능하게 한다.
○ 확장성
레이더 센서와 AI 및 센서 융합을 함으로써 병원, 양로원 및 가정에서 생체 신호 측정과 같은 건강 관리 환경을 구축 할 수 있다.
이는 레이더를 야간등, 스마트폰, 태블릿, 스마트 알람 시계 같은 일상적인 가전 및 전자/전기 제품에 유연하게 장착 될 수 있고, 스마트 홈 디바이스로서 환자 및 장년층을 대상으로 건강 관리 기능을 제공 할 뿐만 아니라 보안용 기능을 동시에 활용 할 수 있음을 의미한다.
○ 작은 크기와 익명성
레이더의 특징은 견고함, 구성 및 장착의 단순함, 그리고 제품의 소형화다.
레이더는 온도의 변화에 강하고 빛의 밝기 및 습도의 변화와 먼지의 영향과 같은 다양한 환경 변화 및 가혹한 조건에서 안정적으로 동작 할 수 있다.
또한 비전도성 물성 커버 뒤에 숨길 수 있으므로, 최종 사용자에게 보이지 않게 할 수 있다.
또 다른 장점으로, 레이더는 개인정보 및 확인을 위한 데이터를 수집하지 않는다.
따라서 이미센 센서나 마이크로폰과 달리 사생활 침해 및 개정정보 유출을 방지할 수 있다.
또한 레이더는 센서 제품의 소형화가 가능하다. 대표적으로 인피니언의 XENSIV™ 60GHz 레이더 센서 BGT60UTR11AIP는 크기가 16㎟에 불과하다.
모든 필요한 부품들을 더하더라도 보드 상으로 2㎠ 미만의 공간만을 차지하므로 컴팩트한 디바이스를 설계할 수 있다.
■ 비접촉 생체 모니터링을 활용할 수 있는 애플리케이션들
○ 병원
병원에서 비접촉 생체 신호 모니터링을 활용해서 환자 치료를 향상시킬 수 있다. ICU, 수술실, 일반 병동, 응급실, 수면 센터 같은 곳에서 유용하게 활용될 수 있다.
레이더 센서를 활용함으로써 예를 들어서 ICU에서 비접촉 방식으로 환자의 생체 신호를 지속적으로 모니터링 할 수 있다.
특히 마취의사와 수술 팀이 수술실에서 환자의 생리적 반응을 실시간으로 면밀하게 모니터링할 수 있다.
더불어 일반 병동에서 비접촉 생체 신호 모니터링을 활용하면 수시로 사람이 직접 생체 신호를 측정할 필요가 없다.
이를 통해 환자는 밤에 더 편하게 수면을 취하고 더 정확하고 신뢰할 수 있는 생체 신호 데이터를 얻을 수 있다.
○ 생활 보조 시설 및 양로원
생활 보조 시설이나 양로원에서는 실시간 모니터링을 활용해서 필요할 때 즉시 개입할 수 있다.
환자의 기준 생체 신호로부터 크게 변화를 일으키면 자동으로 의료진에게 경보를 울릴 수 있다.
또한 레이더 센서는 거주자의 움직임 패턴, 걸음걸이, 자세 변화까지도 감지하고 신속하게 개입할 수 있다.
의사는 대면 방문이 필요 없이 환자에게 연락하고, 진찰하며, 약을 처방하면서 간호사를 보낼 수도 있다.
■ 레이더 센서 기술의 진화
머신러닝, 데이터 융합 및 변수 적응형 필터 등을 사용해서 레이더 센서의 기능성이 높아지고 있다.
머신러닝 알고리즘을 통해 반복적인 패턴을 학습하고 복합적인 데이터 등으로부터 잡음(Noise)를 제거하는 것에 뛰어나다.
머신러닝 알고리즘을 사용해서 원치 않는 잡음으로부터 표적하는 생체 신호를 효과적으로 분리시킴으로써 감지 정확도를 높일 수 있다.
싱가포르의 SCALE이 실시한 연구에 따르면, mm-Wave FMCW 레이더 기반 비접촉 생체 신호 모니터링 시스템에 머신러닝을 적용함으로써 외부 잡음을 손쉽게 필터링하고 해당 생체 지표 정보의 정확성을 높이는 것으로 확인되었다[8].
다중의 레이더 센서들로부터 정보를 융합함으로써(데이터 융합) 향상된 모니터링 기능들을 추가할 수 있다[3].
레이더 센서에다 광학 센서나 가속도계를 결합함으로써 더 포괄적이고 정확한 데이터 모니터링을 달성할 수 있다.
이것은 의료진이 개인의 생체 지표를 더 전체적으로 파악하도록 함으로써 환자를 더 잘 치료하도록 한다.
방해신호(clutter)를 피하고 신호 품질을 높이기 위해서 변수 적응형 필터를 사용 할 수 있는데, 주로 사용되는 두 가지 알고리즘이 LMS(Least Mean Square) 알고리즘과 RLS(Recursive Least Square) 알고리즘이다.
이들 알고리즘을 사용해서 레이더 데이터로 잡음과 간섭을 억제할 수 있다[5].
CFAR(Constant False Alarm Rate) 검출과 Adaptive Beamforming 같은 필터 기법들을 사용할 수도 있다. 이러한 기법들은 임계 수준에서 환경(background) 잡음을 추가적으로 더 낮출 수 있다[6].
추가적으로 레이더 센서가 다중의 채널을 보유하면 여러 사람의 생체 신호를 병렬로 측정할 수 있다.
이 능력은 병원과 양로원을 넘어서 더 다양한 영역에 레이더 센서를 활용할 수 있도록 한다. 예를 들어서 자동차로 이 능력을 활용해서 운전자와 교체 운전자의 안전을 높일 수 있다.
다채널 밀리미터파(Multi-Channel mm-Wave) 레이더는 운전자/교체 운전자를 연속적으로 모니터링함으로써 심장 발작이나 여타의 심폐 이상이 발생되는 징후를 조기에 감지할 수 있다.
이러한 기법들을 어떻게 사용할지 결정하는 것은 특정 레이더 시스템의 필요, 신호 특성, 필요로 하는 생체 신호 같은 것에 따라서 달라질 것이다.
■ 과제와 고려사항
레이더 센서 측정의 정확도와 신뢰성은 다양한 요인들에 의해서 영향을 받을 수 있다. 레이더 센서의 중요한 두 가지 과제와 해결 방법을 알아보자.
○ 인체 움직임의 진폭
신체 활동이나 발작 등으로 인한 빠른 인체 움직임은 레이더 신호로 왜곡을 일으킴으로써 정확한 데이터 추출을 어렵게 할 수 있다. 예를 들어서 걷고 있을 때는 호흡으로 인한 미세한 흉벽 움직임과 다리와 팔을 크게 움직임으로 인한 심장 박동을 구분하기가 어렵다.
이러한 문제를 극복하기 위해서 적응형 필터, Kalman 필터, Particle 필터 같은 알고리즘을 기반으로 한 향상된 모션 보상 기법들을 사용할 수 있다[6].
이러한 기법들은 모션으로 인한 영향을 계산하고 보정함으로써 생체 신호를 더 정확하게 추출하도록 한다.
○ 주기적 캘리브레이션/검사
레이더 센서는 시간이 지나면서 노후화, 환경적 조건, 부품 성능 저하 등으로 인해서 잘못된 생체 지표 리딩을 발생시킬 수 있다.
그러므로 정확도를 유지하기 위해서 주기적으로 캘리브레이션을 실시하고 필요한 조정을 해서 리딩이 허용 한계 이내로 유지되도록 해야 한다.
부가적으로 다음과 같은 방법들이 정확도와 신뢰성을 향상시키기 위해서 도움이 될 수 있다.
- 외부적 간섭을 최소화하고 신호 품질을 극대화하기 위해서는 레이더 센서를 안정적이고 적절한 장소에다 놓아둔다.
- 레이돔(레이더 돔) 기술을 사용해서 밀리미터파 레이더 센서 및 안테나를 비, 햇빛, 바람 같은 외부적 환경의 영향으로부터 보호한다.
- 측정 결과를 기존 측정 기법과 비교해서 신뢰성을 평가하고 개선할 부분이 있는지 확인한다.
머신 러닝 및 딥 러닝 알고리즘을 활용해서 대규모 데이터셋으로부터 패턴과 상관성을 학습함으로써 견고한 측정을 달성할 수 있다.
■ 인피니언의 XENSIV™ 60GHz 레이더 센서를 활용한 레이더 센싱 향상
인피니언의 밀리미터파 레이더 포트폴리오는 다양한 IoT 및 차량 애플리케이션에 사용하도록 FMCW 및 도플러 레이더 센서들을 제공한다.
▲그림 2 : XENSIV™ 60GHz BGT60TR13C
▲그림 3 : 인피니언의 진보된 레이더 센서인 XENSIV™ 60GHz BGT60UTR11AIP
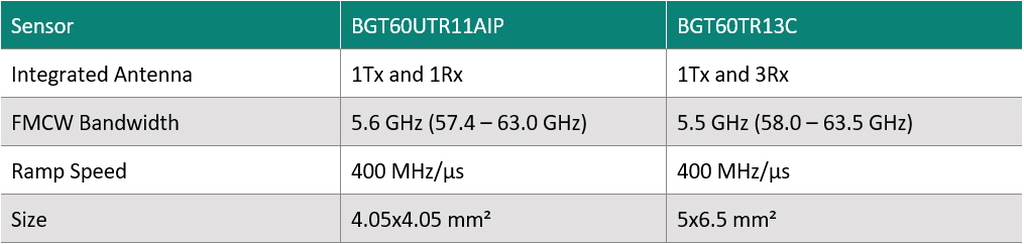
원격 생체 신호 모니터링 시스템 용으로 이들 센서의 제품 특징을 알아보자.
○ 고유의 패키지 디자인
이들 레이더 센서는 각기 분리형 (Discreteness) 디자인으로 생체 신호 모니터링을 간접적으로 가능하게 한다.
BGT60TR13C 레이더 센서는 L 형태 AIP이고, BGT60UTR11AIP 레이더 센서는 U 슬롯 AIP이다. 두 디자인 모두 컴팩트한 폼팩터로 효율적인 안테나 통합을 가능하게 한다. 또한 이들 센서는 소형 패키지로 설계 시에 PCB 면적을 절약하고 전반적인 설계를 간소화하도록 한다.
※ 비고 : AIP(Antenna in Package) 기술은 IC 패키지 내로 하나 혹은 그 이상의 안테나를 내장한 안테나 패키징 솔루션을 말한다.
▲표 1 : 이들 XENSIV™ 60GHz 레이더 센서의 차이점
○ FSM(Finite-state machine) 내장
비접촉 생체 신호 측정을 위해서 한 가지 중요한 과제는 환자가 변칙적인 인체 움직임을 보일 때 네트워크 자가 치유(network-self-healing) 메커니즘을 가능하게 하는 것이다.
BGT60TR13C와 BGT60UTR11AIP는 FSM (Finite-state machine)에 기반한 자율 커넥티비티 복구 알고리즘을 사용해서 이 문제를 해결한다.
이들 레이더 센서는 FSM을 내장함으로써 Chirp을 생성하고, Data를 획득하며, 메모리에 저장하는 과정을 자율적으로 수행할 수 있다.
어떠한 비정상적 노드가 발생되면 중요도가 높지 않으면서 가장 가까이에 있는 노드로 대체해서 매끄럽게 네트워크 커넥티비티를 복구한다[7].
이와 같이 최적화된 전원 스위칭 메커니즘을 사용해서 Duty-cycle 을 조절하면서 전력 소모(avg. xx mW)를 최소화한다.
DC 듀티 사이클링을 통해서 추가적으로 전력을 절약할 수 있다.
○ 광대역 주파수 사용
이들 센서는 믿을 수 없을 만큼 극히 넓은 대역폭(최대 5.6GHz)과 높은 거리 분해능(∼3㎝)으로 최대 15미터 거리로 ㎜ 정확도로 미세한 움직임을 감지할 수 있다.
이러한 능력은 심장 발작을 조기에 감지하고 상태가 심각하거나 집중 치료를 받고 있는 환자들의 생리적 상태를 모니터링하기 위해서 중요하다.
의료진이 이러한 상세한 정보를 활용해서 치료 계획을 맞춤화하고 개개인에 맞는 약물을 처방할 수 있다. 그럼으로써 심각한 상태를 완화하는 데 도움이 된다.
○ 사용의 용이성
높은 SNR(신호대 잡음비)로, 다른 장치들로부터 감지를 방해하는 복잡한 환경이라 하더라도 레이더 센서는 긴 거리에 있는 대상의 움직임도 감지할 수 있다.
BGT60TR13C와 BGT60UTR11AIP 둘 다 높은 SNR로 설계됨으로써 미세한 흉벽 움직임을 감지할 수 있다.
이들 레이더 센서는 의복, 침구, 여타의 비금속 장애물을 통과해서 생체 신호를 감지할 수 있을 뿐만 아니라 복잡한 장치를 추가적으로 필요로 하지도 않고, 환자가 옷을 벗을 필요도 없기 때문에 병원이나 양로원 같은 다양한 곳에서 환자 모니터링에 활용하기에 유용하다.
■ 맺음말
레이더 기술은 피부에 접촉할 필요 없이 비침습적으로 연속적으로 생체 신호 모니터링이 가능하다.
레이더 센서를 활용한 생체 신호 모니터링은 손쉽게 사용하면서 에너지를 절약하고, 정확한 자신의 생체 데이터를 제공함으로써 본인을 모니터링하고자 하는 노인이나 개인들에게 특히 유용하다.
이
링크에서 인피니언의 앞선 레이더 센서인 XENSIV™ 60GHz BGT60UTR11AIP에 관한 더 자세한 정보를 볼 수 있다.
※ 참고문헌
[1] Weller RS, Foard KL, Harwood TN. Evaluation of a wireless, portable, wearable multi-parameter vital signs monitor in hospitalized neurological and neurosurgical patients. J Clin Monit Comput [Internet]. 2018 [cited 2023 May 30];32(5):945-51. Available from: https://pubmed.ncbi.nlm.nih.gov/29214598/
[2] Balasubramanian V, Vivekanandhan S, Mahadevan V. Pandemic tele-smart: a contactless tele-health system for efficient monitoring of remotely located COVID-19 quarantine wards in India using near-field communication and natural language processing system. Med Biol Eng Comput [Internet]. 2022;60(1):61-79. Available from: http://dx.doi.org/10.1007/s11517-021-02456-1
[3] Moshawrab M, Adda M, Bouzouane A, Ibrahim H, Raad A. Smart wearables for the detection of occupational physical fatigue: A literature review. Sensors (Basel) [Internet]. 2022 [cited 2023 May 27];22(19):7472. Available from: http://dx.doi.org/10.3390/s22197472
[4] Barreto-Cubero AJ, G?mez-Espinosa A, Escobedo Cabello JA, Cuan-Urquizo E, Cruz-Ram?rez SR. Sensor data fusion for a mobile robot using neural networks. Sensors (Basel) [Internet]. 2021 [cited 2023 May 27];22(1):305. Available from: https://www.mdpi.com/1424-8220/22/1/305
[5] Lampl T. Implementation of adaptive filtering algorithms for noise cancellation [Internet]. Diva-portal.org. [cited 2023 May 27]. Available from: https://www.diva-portal.org/smash/get/diva2:1456739/FULLTEXT01.pdf
[6] Wolff D-I (fh) C. False alarm - radartutorial [Internet]. Dipl.-Ing. (FH) Christian Wolff. [cited 2023 May 27]. Available from: https://www.radartutorial.eu/01.basics/False%20Alarm%20Rate.en.html
[7] Zhang Y, Wang J, Hao G. An autonomous connectivity restoration algorithm based on finite state machine for Wireless Sensor-Actor Networks. Sensors (Basel) [Internet]. 2018 [cited 2023 May 30];18(1):153. Available from: https://www.mdpi.com/1424-8220/18/1/153
[8] Iyer S, Zhao L, Mohan MP, Jimeno J, Siyal MY, Alphones A, et al. mmWave radar-based vital signs monitoring and arrhythmia detection using machine learning. Sensors (Basel) [Internet]. 2022 [cited 2023 Jun 15];22(9):3106. Available from: https://www.mdpi.com/1424-8220/22/9/3106
[9] Herbst E, Metzler TJ, Lenoci M, McCaslin SE, Inslicht S, Marmar CR, et al. Adaptation effects to sleep studies in participants with and without chronic posttraumatic stress disorder: Adaptation effects to sleep studies and PTSD. Psychophysiology [Internet]. 2010 [cited 2023 Jul 17];47(6):1127-33. Available from: http://dx.doi.org/10.1111/j.1469-8986.2010.01030.x